eye disorders
- related: Medicine
Eye disorders
- Blepharospasm
- orbital cellulitis
- optic neuritis
- eye problems
- uveitis conjunctivitis keratitis
- choroidal melanomas
- glaucoma
Hordeolum
Hordeolum (stye) is a bacterial infection of the sebaceous glands in the eyelid. Patients have tenderness, redness, and swelling at the eyelid margins. Hordeolum is not a complication of bacterial conjunctivitis.
Hordeolum is the acute obstruction of the meibomian gland, eyelash follicle, or lid-margin tear gland, with associated inflammation and possible Staphylococcus aureus infection. It does not result in inflammation of the globe itself.
Uveitis
Examination findings in anterior uveitis can include hyperemia concentrated at the junction of the sclera and cornea (ciliary flush), pupillary constriction, a hazy "flare" in the aqueous humor, and layering of white cells in the anterior chamber (hypopyon).
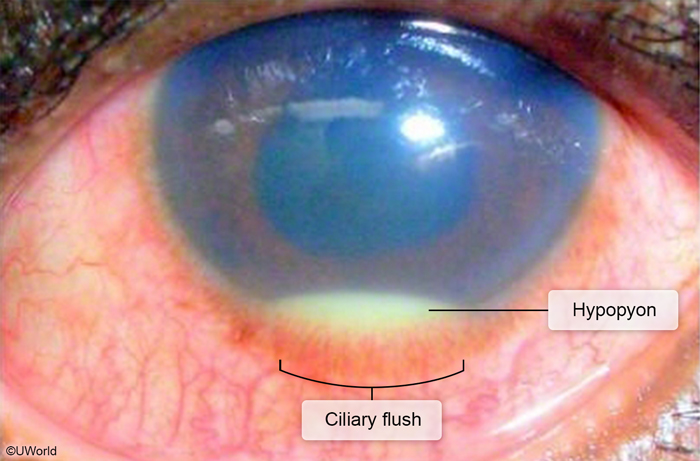
The presence of leukocytes in the anterior chamber is diagnostic of anterior uveitis and differentiates it from other causes of red eye. Anterior chamber flare is another common manifestation and is created by extravasated protein that causes dispersal of light on slit lamp examination. Patients with suspected uveitis warrant expedited ophthalmology consultation. Topical corticosteroids are the treatment of choice for noninfectious uveitis.
Episcleritis
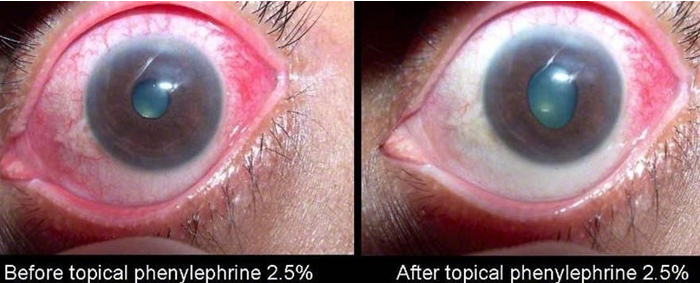
Episcleritis does not commonly present with pain but rather with erythema and tearing. Vision remains unimpaired.
Common Vision Problems
Refractory vision abnormalities are conditions that affect the focal point of vision relative to the retina. They include myopia, hyperopia and astigmatism.
Myopia, commonly known as nearsightedness, is a condition where the refracting power of the eye is greater than normal. This places the focal point of the eye anterior to the retina.
Hyperopia, commonly known as farsightedness, is a condition where the refracting power of the eye is less than normal. This places the focal point of the eye posterior to the retina.
Astigmatism is a condition where the corneal surface is asymmetric, which causes inconsistent refraction of light into the eye. This results in blurred vision.
Refractory vision abnormalities present with blurred vision. Myopia worsens as the object gets farther away, while hyperopia worsens when the object gets closer.
Refractory vision abnormalities are treated with corrective lenses. Myopia and hyperopia can also be corrected surgically.
Strabismus, also known as heterotropia, is a condition of the eye where an abnormal alignment is not able to be overcome by normal motor control.
Patients with strabismus will demonstrate a gaze for each eye that is in different directions. This results in double vision and progressive blindness. If untreated, the visual information from the misaligned eye can be suppressed, leading to amblyopia, which is discussed below.
Strabismus is treated with vision training, with surgery often required to align the eyes bilaterally.
Amblyopia, also known as lazy eye,is the result of a developmental defect in the neural pathways of the eye.
Patients with amblyopia will have poor visual acuity and spatial differentiation in the affected eye.
Amblyopia is treated with either patching or atropine drops. Patching is usually preferred by parents due the anticholinergic effects of atropine.
Presbyopia is an age-related disorder that is caused by the loss of lens elasticity and concomitant loss of accommodating power.
Patients with presbyopia experience difficulty reading at close range and thus have a classic history of holding reading materials at arm's length.
Pupil
Argyll Robertson pupil is a condition where the patients pupil does not constrict in response to light, but does constrict in order to accommodate to near objects. It accommodates but does not react.
A common association/cause of Argyll Robertson pupil is syphilis, which is why it is also known as “prostitutes pupil.” Other causes includes SLE and DM.
Marcus Gunn pupil is a condition where light shined in the affected pupil produces a markedly smaller consensual light reflex than when shined in the normal pupil. This can be tested with the “swinging flashlight test.” The examiner shines a light into the normal eye, causing both pupils to constrict. The examiner then swings the light to the abnormal eye. Damage to the afferent fibers of cranial nerve II in Marcus Gunn pupil means that less light is perceived, and neither pupil will constrict.
The cause of Marcus Gunn pupil is an afferent nerve defect, commonly the optic nerve.
Horner syndrome is the combination of ptosis, miosis, and anhidrosis.
The cause of Horner syndrome is a sympathetic trunk lesion, a common etiology of which is a pancoast tumor.
Adie Pupil
Adie Pupil is a condition where the patients pupil is tonically dilated and responds slowly to light.
The cause of Adie pupil is damage to the parasympathetic innervation to the iris.
MLF syndrome
MLF (medial longitudinal fasciculus) syndrome is a condition affecting lateral gaze where the abduction of one eye is not paired with adduction of the contralateral eye.
The cause of MLF syndrome is damage to the medial longitudinal fasciculus, which is commonly seen in MS and intracranial lesions.
Renal artery
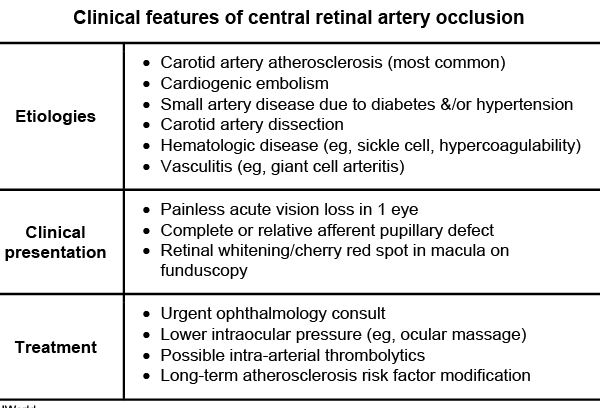
This patient's presentation—acute, painless monocular vision loss—suggests central retinal artery occlusion (CRAO), which usually affects patients age >60 with underlying cardiovascular risk factors. CRAO is most commonly due to carotid atherosclerosis as the central retinal artery is a branch of the ophthalmic artery, which arises from the internal carotid artery. Other etiologies include cardiac embolism, small vessel disease (eg, hypertension, diabetes), and vasculitis (eg, giant cell arteritis). Funduscopic examination usually shows diffuse ischemic retinal pallor and a cherry red spot at the macula (due to preserved circulation via posterior ciliary arteries). Evaluation includes laboratory studies to exclude giant cell arteritis (erythrocyte sedimentation rate, C-reactive protein), carotid artery imaging, and cardiac evaluation in patients with a suspected cardioembolic source.
CRAO can cause irreversible retinal damage within 90-100 minutes. As a result, patients require urgent ophthalmology consultation and interventions to lower intraocular pressure (eg, ocular massage, anterior chamber paracentesis, intravenous acetazolamide or mannitol). Long-term management includes atherosclerotic risk factor modification (lipid-reducing and antiplatelet agents) for prevention of recurrent vascular events. Prognosis is poor in patients with severe vision loss at the time of presentation.
Central retinal vein occlusion can also present with painless, acute, or subacute monocular vision loss. Central retinal vein occlusion is usually due to nonembolic causes. Examination can show tortuous and dilated veins, diffuse hemorrhages, disk swelling, and cotton wool spots.